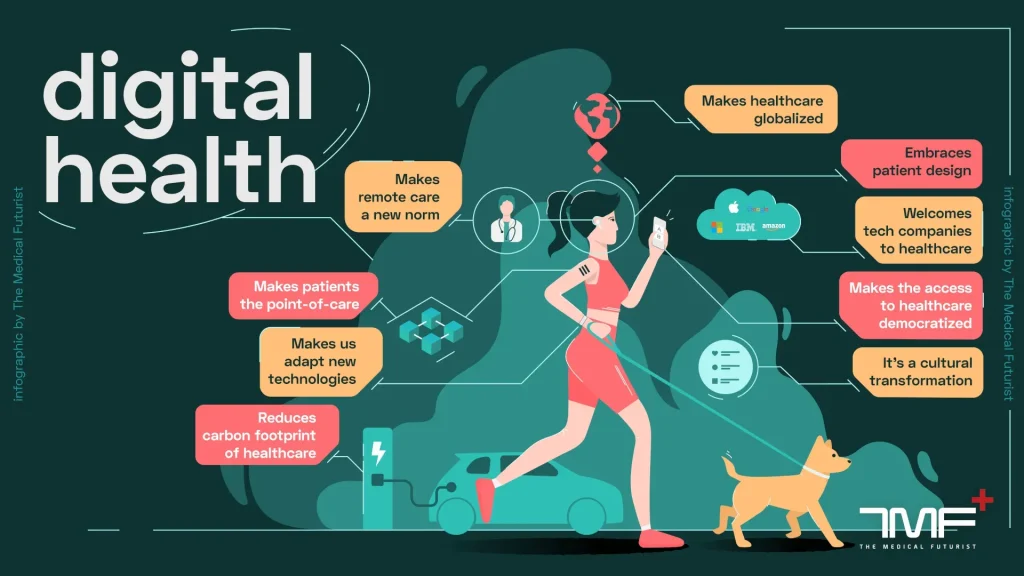
digital health is reshaping how individuals monitor, interpret, and manage well-being in today’s care landscape, shifting care from episodic treatment to proactive, continuous engagement that follows people through daily routines, work, travel, and moments of decision, inviting them to participate at their own pace and adapt to changing circumstances, and this inclusive approach respects diverse needs, literacy levels, and cultural contexts, ensuring tools are usable by beginners and tech-savvy users alike. With health apps enabling daily tracking of activity, nutrition, and mood and with the growth of patient-friendly interfaces, this ecosystem turns data into actionable guidance that supports healthier habits, motivates consistency, enables clinicians to tailor recommendations to changing circumstances, and fosters lasting motivation through gamified progress, social support, and personalized nudges, and ease of integration into daily routines. Wearable devices extend this insight with real-time metrics on activity, sleep, and vital signs, creating a bridge between at-home monitoring and clinical decision-making while also highlighting trends that inform preventive strategies and personalized coaching, which can be interpreted at a glance and shared with care teams to inform adjustments to therapy. Telehealth expands access to clinicians, sustains follow-up, and reduces the friction of in-person visits, making care more convenient without sacrificing quality, and it fosters ongoing collaboration across time zones, routes of care, and diverse patient needs, and supports cooperative management plans that align with patient goals, across multidisciplinary teams including nurses, pharmacists, and care coordinators. As health data privacy concerns are addressed through privacy-by-design practices, consent clarity, and robust security, trust grows and more people feel comfortable participating in this evolving health tech landscape, knowing their information is protected and used to support better outcomes, this helps address concerns about consent, data minimization, and auditability in everyday use, and governance reviews to ensure ongoing privacy protection.
Beyond the shorthand for the broader health-tech movement, the topic is framed through terms like e-health, mHealth, and health technology to describe a broader toolkit for care delivery. From remote patient monitoring and telemedicine to interoperable records and cloud-based analytics, the semantic field emphasizes connected systems that support informed decisions without overwhelming patients. User-centered design, robust data governance, and privacy-by-design principles remain essential as tools scale from smartphones to biometric sensors and clinician dashboards. In this framing, the focus shifts from individual devices to an integrated care stack where technology, clinical expertise, and policy work in concert to expand access, improve outcomes, and enhance the care experience.
Digital Health in Everyday Life: Leveraging Health Apps and Wearable Devices for Smarter Care
Digital health tools fuse health apps and wearable devices to support everyday decisions. Health apps help track activity, sleep, nutrition, and mental well being, while wearables continuously collect data on heart rate, steps, and other biomarkers. When used thoughtfully, these tools translate streams of information into practical insights, revealing patterns such as late night activity, fluctuating energy, or periods of stress. This enables small, sustainable changes like hydration prompts, movement reminders, or targeted sleep strategies, and provides a data rich view that clinicians can review to tailor care. They also complement telehealth by supplying patient generated data for remote consultations.
Beyond individual use, aggregated app and wearable data contribute to population health insights and remote monitoring. Interoperability with electronic health records allows clinicians to see a holistic view of overall patient health, enabling personalized recommendations that fit real-life routines. The result is a complementary model of care where technology-backed feedback supports both telehealth and in-person care, guided by evidence and designed to respect user privacy and autonomy.
Telehealth, Health Data Privacy, and Interoperability: Building Trust in Digital Health
Telehealth expands access and convenience by enabling video visits, secure messaging, and asynchronous symptom checks. When paired with health apps and wearable data, clinicians can monitor chronic conditions more closely, adjust treatment plans sooner, and maintain continuity of care even when in person visits are not feasible. This convenience must be balanced with clear privacy protections including consent, data encryption, and robust access controls across platforms.
Interoperability and governance are essential to trustworthy digital health. Seamless data flow between health apps, wearable devices, and electronic health records creates a consolidated, real-time picture of patient health with less duplication and confusion. Privacy-by-design practices, ongoing security audits, and patient control over data sharing help build confidence in telehealth and analytics, supporting better outcomes, higher engagement, and sustainable adoption of digital health solutions.
Frequently Asked Questions
How do digital health tools like health apps and wearable devices work together to support everyday care?
Digital health combines software tools (health apps), hardware (wearable devices), and care models to empower daily health management. Health apps track activity, sleep, nutrition, mood, and chronic-condition data, while wearables provide continuous metrics such as heart rate and sleep quality. Together, they generate insights, enable personalized feedback, and support remote monitoring, complementing traditional care and helping clinicians review trends to adjust plans as needed.
Why is health data privacy essential in digital health and telehealth, and what should users look for in privacy‑friendly tools?
Health data privacy is foundational in digital health and telehealth. Look for tools that follow privacy-by-design principles, clear consent, data ownership information, and robust security (encryption, access controls, regular audits). Seek transparent data practices, options to share or export data, and clear explanations of how data may be used (such as for improving algorithms or de-identified research). Ensure telehealth data integrates with your electronic health records in a secure, user-consented manner.
| Aspect | Key Points | Impact / Benefits |
|---|---|---|
| The Power of Health Apps | Entry point to digital health; range from step counters to mood journals and dashboards; supports daily habits and timely actions. | Translates data into insights; supports motivation; guides discussions between users and clinicians; enables behavior change. |
| Wearable Devices and Continuous Insight | Collect data on activity, heart rate, sleep; real-time feedback; trend analysis; goal setting. | Supports personal health management; enables early detection and remote monitoring; bridges clinic and home for responsive care. |
| Telehealth: Access, Convenience, and Continuity of Care | Video visits, secure messaging, asynchronous symptom checks; reduces travel and wait times; improves care continuity. | Improved chronic condition management; expanded access to mental health care; data integrated with EHR for informed decisions. |
| Health Data Privacy and Security | Trust-based foundation; privacy by design; informed consent; data ownership and sharing policies; encryption and audits. | Builds user confidence; supports responsible data use in research; reduces risk of breaches. |
| Practical Integration | Start with one app and one wearable; choose evidence-based features; review privacy settings; discuss with clinician; emphasize interoperability. | Improves data utility; enables personalized interventions; supports sustainable adoption. |
| Challenges and Considerations | Accessibility and digital literacy gaps; disparities due to internet access or devices; data quality and device limitations; governance needs. | Addresses equity concerns; mitigates misinterpretation; sets realistic expectations and safeguards. |
| A Practical Roadmap for Readers | Define health goals; start small; protect privacy; consult clinician; evaluate impact. | Provides actionable steps to implement digital health tools and measure outcomes. |
Summary
Digital health is a broad, evolving landscape where apps, wearables, telehealth, and privacy-conscious data practices come together to support healthier lives and more patient-centered care. This descriptive overview highlights how health apps translate data into actionable insights, how wearables enable continuous monitoring, and how telehealth expands access while privacy and interoperability build trust. Effective digital health requires practical integration: choosing evidence-based tools, safeguarding privacy, ensuring data flows between devices and electronic health records, and collaborating with clinicians. When designed with equity and quality in mind, digital health can improve prevention, chronic disease management, and health outcomes across diverse populations.